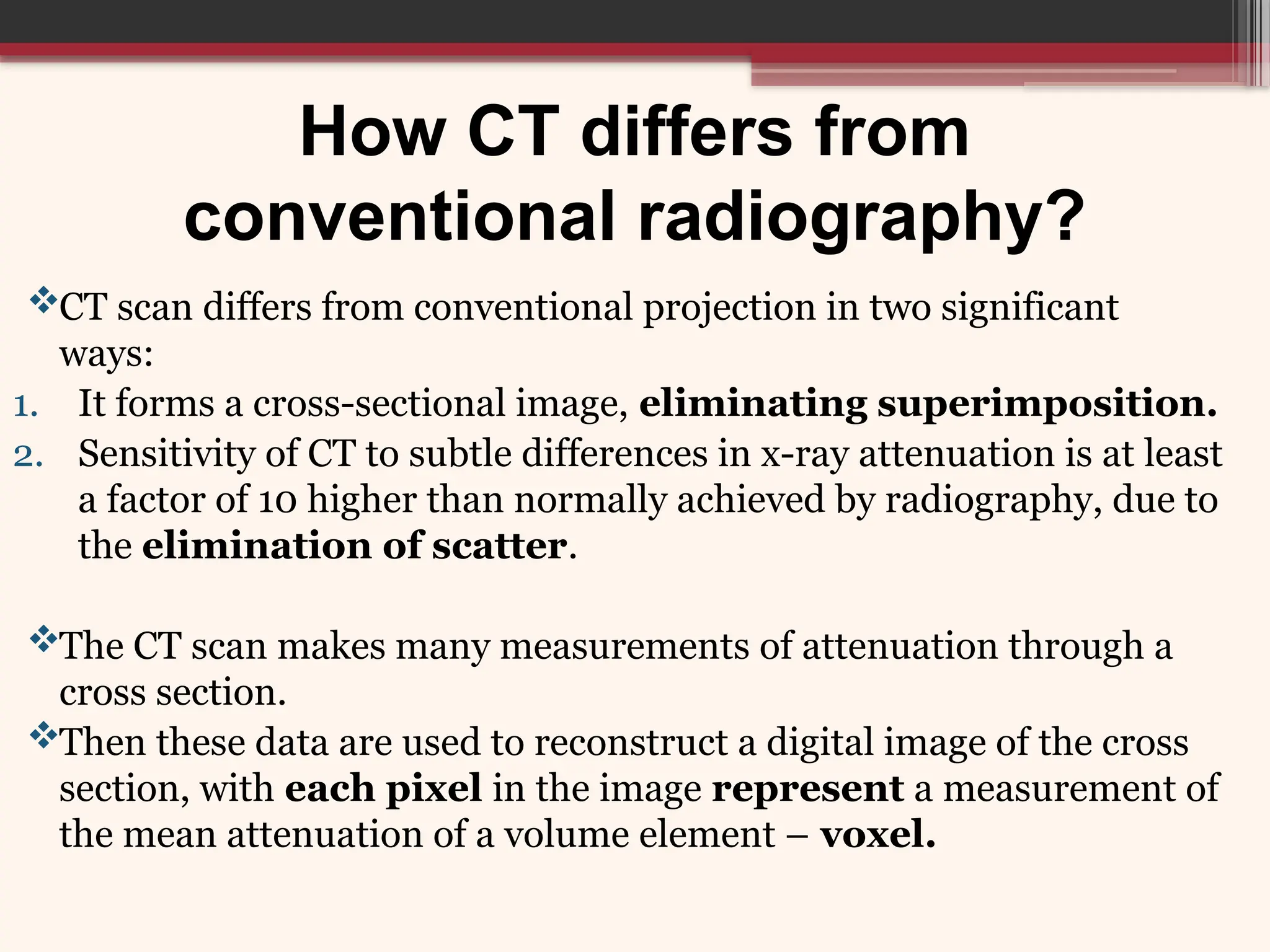
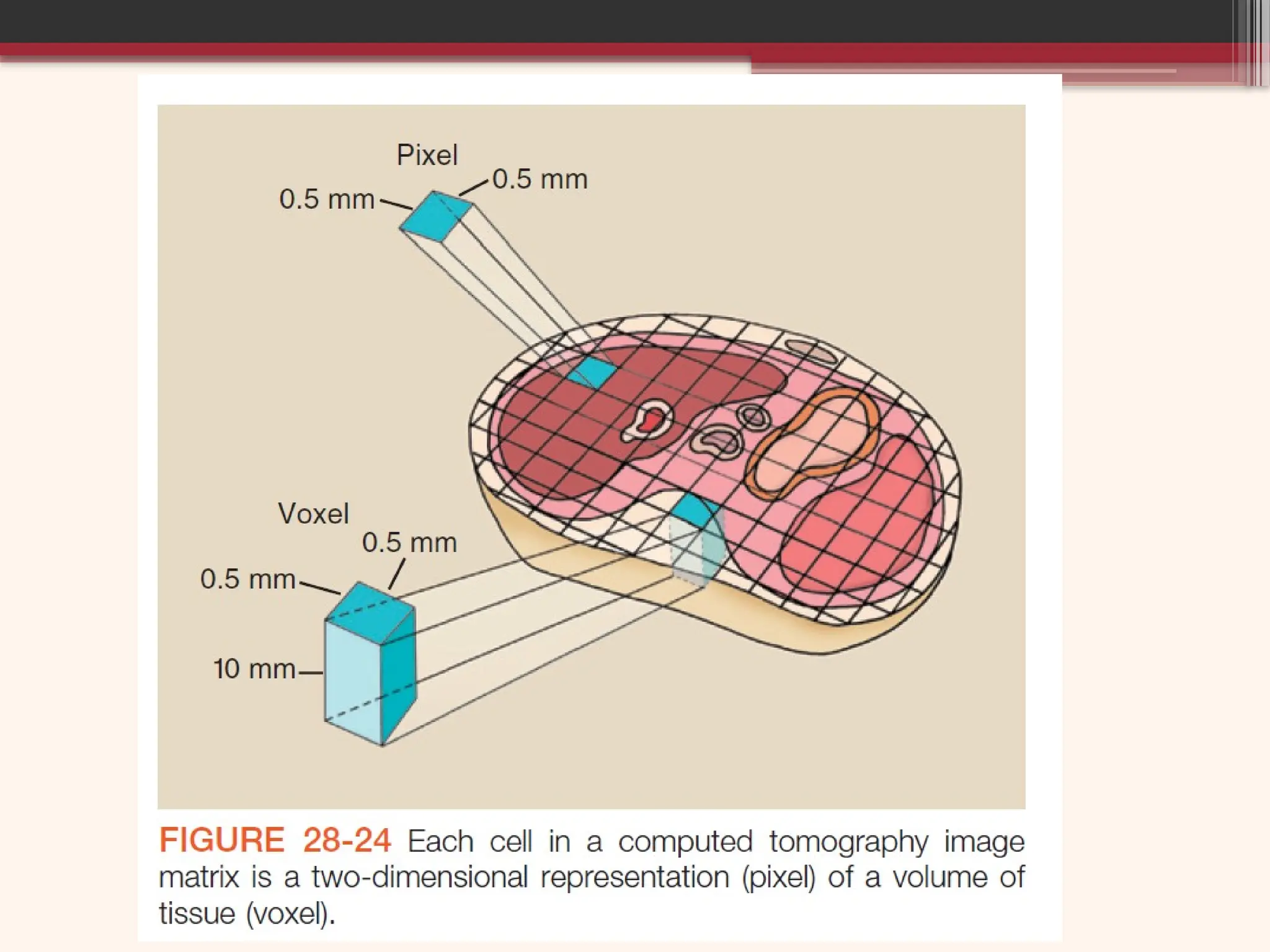
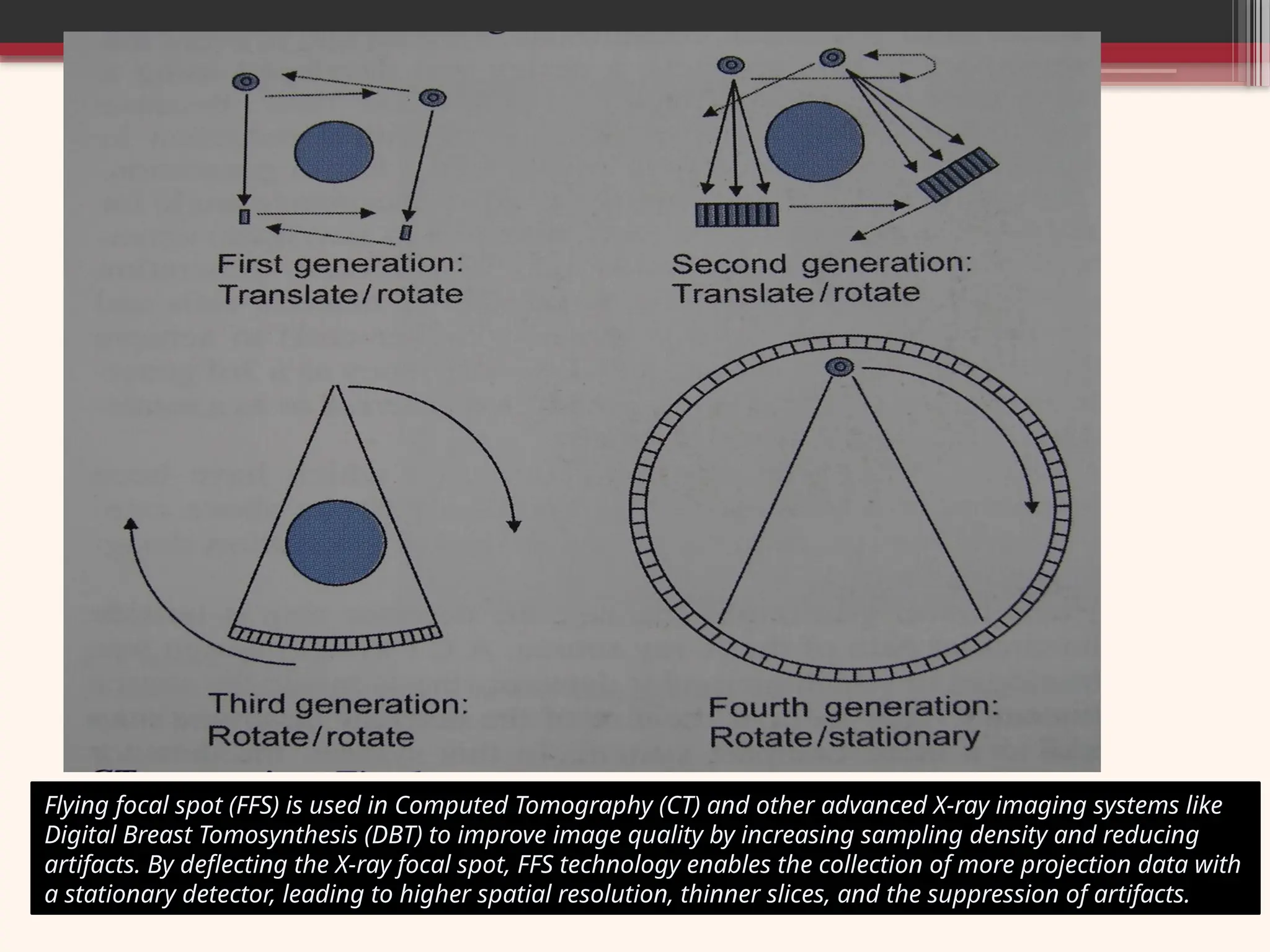
Greek words: Tomos (cut/slice/section) and Graphein (write/record). Literal definition: A form of tomography (imaging technique to provide cross sectional images of the body) in which a computer controls the motion of the X-ray source and detectors, processes the data, and produces the image. Computed Tomography is fundamentally a method of acquiring and reconstructing an image of a thin cross section of an object. CT is a technique of creating tomographic images from digitized data obtained by exposing the patient to x-rays from many different angles. In this presentation, we start from one of the greatest discovery in the history of mankind the CT scan and how we have evolved to reach the current level of modern CT imaging in the world of radiology.
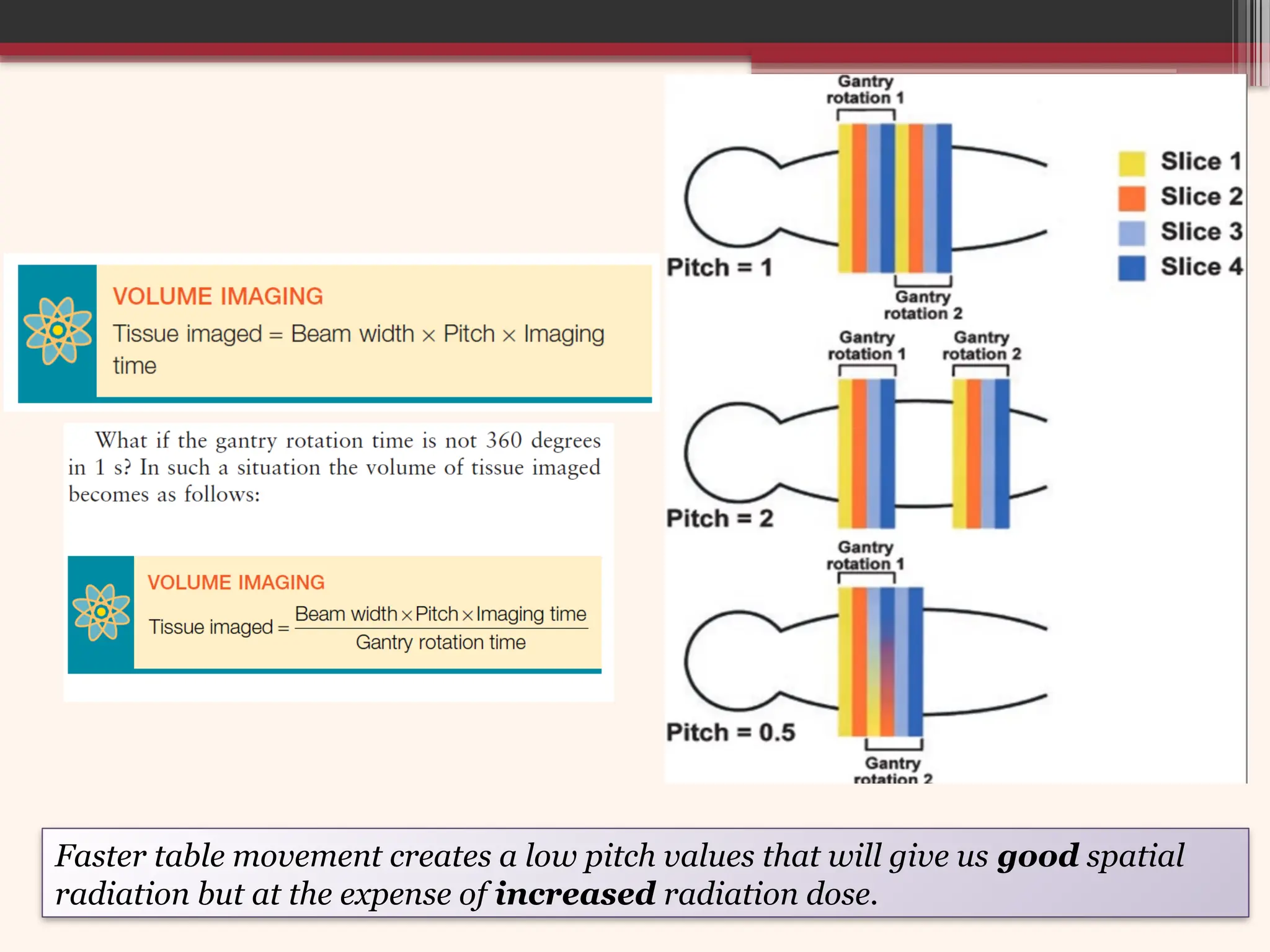
In slide no. 60, regarding pitch typographical error is corrected as "Slower table movement creates a low pitch values that will give us good spatial resolution but at the expense of increased radiation dose."