Abstract
Aims/hypothesis
The aim of this work was to compare the cardiopulmonary, sympathoadrenal and metabolic responses to physical exercise in adults with type 1 diabetes with or without cardiovascular autonomic neuropathy (CAN).
Methods
Data collected during a graded maximal exercise test (GXT) from 24 participants with type 1 diabetes and CAN were compared against 24 matched control individuals without CAN (NO CAN). Throughout exercise, integrated cardiopulmonary variables were obtained continuously via spiroergometry. Plasma concentrations of adrenaline (epinephrine), noradrenaline (norepinephrine), glucose (PG) and lactate (PLa) were measured in 3 min intervals during exercise as well as at the peak workload. Data were assessed via independent t tests and two-factor ANOVAs with significance accepted at p≤0.05.
Results
Participants with CAN displayed a reduced \({\dot{V}\text{O}}_{2\text{peak}}\) (CAN 19.6 ± 5.4 vs NO CAN 27.5 ± 7.8 ml kg−1 min−1) as well as attenuations in several other cardiopulmonary, lactate and exercise performance variables during GXT. Peak catecholamine concentrations were lower in CAN vs NO CAN (AD 0.17 ± 0.12 vs 0.38 ± 0.27 ng/ml, p=0.002; NAD 1.86 ± 1.04 vs 2.85 ± 1.23 ng/ml, p=0.007) as were the magnitudes of change in hormonal concentrations from rest to peak workloads (adrenaline Δ +0.13 ± 0.12 vs Δ +0.32 ± 0.24 ng/ml, p=0.005; noradrenaline Δ +1.33 ± 0.89 vs Δ +2.33 ± 1.30 ng/ml, p=0.005). PG concentrations throughout exercise were similar between groups and remained unchanged from rested values irrespective of CAN status.
Conclusions/interpretation
In adults with type 1 diabetes, CAN was associated with exercise intolerance characterised by impairments in various cardiopulmonary, sympathoadrenal system and metabolic responses to GXT. These data support uncovering the presence of CAN when prescribing a personalised physical training plan.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Cardiovascular autonomic neuropathy (CAN) is a frequent complication of type 1 diabetes affecting approximately 30% of the population [1]. The condition is caused by damage to the autonomic nerve fibres that innervate the heart and blood vessels, increased baroreceptor intima–media thickness, reduced vascular distensibility and endothelial dysfunction [2]. In individuals with type 1 diabetes, the concurrent presence of CAN carries an increased risk of CVD and all-cause mortality [3]. In its early stages, CAN leads to dysfunction of the parasympathetic nervous system with a consequential shift from vagal to sympathetic predominance. An increase in sympathetic tone continues with advancing CAN whereby denervation of sympathetic nerves impairs responsivity to excitatory stimuli [4, 5].
Autonomic nervous system reflexes are important in regulating many cardiovascular and metabolic responses to exercise [6]. Indeed, exercise capacity, often referred to as cardiorespiratory fitness (CRF), is a product of the cardiovascular system’s efficacy in delivering oxygen to exercising skeletal muscle and, consequently, of exercising muscle to extract oxygen from the blood [7]. Independently, CRF is recognised as a powerful predictor of CVD risk and all-cause mortality across a spectrum of age, race, sex and disease state [8,9,10,11,12].
Several studies have documented attenuated CRF and/or abnormal cardiopulmonary and neuroendocrine responses to exercise in individuals with type 1 diabetes relative to those without the condition [13,14,15,16,17]. In most instances, the focal point has been on understanding relationships between glycaemic management and indices of exercise intolerance. Much less explored, and perhaps more nuanced, is the impact of autonomic neuropathy on CRF in those with type 1 diabetes [18, 19]. In data that have been published, details on the specificity of the cardiovascular subtype are absent and/or control groups are not matched in key variables known to influence CRF (i.e. sex, age and BMI). Furthermore, the inclusion of comparative control cohorts of individuals who do not have type 1 diabetes makes for difficulty in disentangling the effects of diabetes, vs CAN, per se. Thus, efforts that seek to deepen our understanding of the impact of CAN when superimposed with type 1 diabetes on the physiological responses to exercise having accounted for confounding variables are important prerequisites for establishing appropriate targeted interventions aimed at improving CRF in high-risk clinical cohorts.
Although we have recently shown that glucose is unlikely to change during graded exercise testing (GXT) in people with type 1 diabetes [20, 21], this conclusion has been drawn from data on individuals without overt autonomic neuropathy, for whom glucose counterregulatory mechanisms and hypoglycaemia awareness were assumed to be intact [22]. Considering the involvement of the autonomic nervous system in regulating glucose homeostasis during exercise, and the potential implications of hypoglycaemia on cardiac vagal outflow [23], profiling glucose levels during exercise in adults with type 1 diabetes with or without CAN is warranted from a safety, if not informative, perspective.
With this in mind, this study investigated and compared the cardiovascular, sympathoadrenal and metabolic responses to GXT in adults with type 1 diabetes with and without CAN.
Methods
Study design and ethical governance
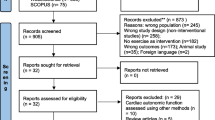
A total of 48 adults with type 1 diabetes took part in this study. Of this cohort, half had established CAN (n=24) and the other half were age- and sex-matched individuals without CAN (NO CAN, n=24). Age matching was done with a maximum allowance of 10 years whilst the sex of participants was determined via self-report. Participants were enrolled in a cross-sectional study from an ongoing neuropathy screening study at Steno Diabetes Center Copenhagen (Herlev, Denmark) [1] and so the sample size was predetermined by the available cohort. The study was conducted according to the Declaration of Helsinki and all procedures were approved by the National Research Ethics Committee of Denmark (H-19029796). All volunteers were provided with a full written and verbal description of the study prior to undertaking any study-related activities. Informed consent was given voluntarily before proceeding with participation.
Inclusion and exclusion criteria
Main study inclusion criteria were as follows: clinical diagnosis of type 1 diabetes as validated via autoantibodies; aged between 18–80 years; BMI of 18.0–33.0 kg/m2; and a definitive diagnosis of either having CAN or not. This was determined by three cardiovascular reflex tests (CARTs) using the handheld instrument Vagus (Medicus Engineering, Aarhus, Denmark): (1) lying to standing test; (2) deep breathing test; and (3) the Valsalva manoeuvre. CAN was diagnosed by the presence of two or more pathological test results while NO CAN status was assigned when all CARTs were normal [24]. One abnormal CART was interpreted as borderline CAN and, hence, these participants were excluded from further involvement due to an inability to be definitively grouped. All CAN testing was performed after 10 min of rest in a supine position in a quiet and isolated examination room. Smoking as well as consumption of food (with an accompanying bolus insulin dose) and caffeinated beverages were prohibited for at least 2 h before testing. Participants were also asked to avoid strenuous physical activity and encouraged to avoid level 2 hypoglycaemia (defined as a fingertip capillary blood glucose value of <3.0 mmol/l) in the 24 h prior to laboratory attendance. Verification of adherence to these preparatory procedures was completed at the screening visit and, in instances where adherence was breached, the visit was rescheduled.
Main exclusion criteria were as follows: female participants who were breast-feeding, pregnant or planning to become pregnant during the trial period; evidence of alcohol or drug abuse; and the presence of any medical or psychological condition that could interfere with study participation and/or an individual’s safety as judged by the clinical members of the investigatory team.
Pre-exercise screening procedures and glycaemic safety monitoring
After successful completion against the main study inclusion criteria, participants were further screened against the American College of Sports Medicine reference guidelines for absolute and relative contraindications to exercise stress testing [25], including clearance of any cardiac abnormalities via a 12-lead ECG by the study physician. A peripheral i.v. cannula was then inserted in the antecubital fossa to obtain baseline characteristics and trial-day venous blood samples. Prior to exercise, participants also completed the Clark hypoglycaemia awareness questionnaire [26].
Fifteen minutes before the anticipated start time of GXT, participants’ plasma glucose (PG) levels were checked from a safety perspective. If, at this point, the glucose value was <5 mmol/l, GXT was delayed and participants consumed 15 g of carbohydrates in the form of dextrose tablets (Dextro Energy, Krefeld, Germany). A second PG measurement was obtained 15 min later, and the process was repeated until PG was above the target threshold (≥5 mmol/l). An equal proportion of participants in each group received supplementary carbohydrates before exercise to reach PG levels deemed ‘safe to start’ (NO CAN n=12 vs CAN n=9, χ2 [1, n=48]=0.762, p=0.383). If the PG concentration was ≥15.0 mmol/l and blood ketone levels were low (<0.6 mmol/l), exercise went ahead at the discretion of the participant with frequent monitoring for ketone body formation. If ketone levels were ≥1.5 mmol/l, the visit was cancelled and rescheduled.
GXT protocol
Participants performed a GXT on a workload-controlled cycle ergometer (Corival, Lode, Groningen, the Netherlands and Monark LC4, Vansbro, Sweden). A predetermined protocol was employed that consisted of a 3 min passive resting phase, a standardised 3 min warm-up phase (20 W), followed by 1 min increases in workload until volitional exhaustion. Volitional exhaustion was defined by one or more of the following parameters: (1) an inability to maintain a pedalling cadence of >50 rev/min for >5 s; (2) a respiratory exchange ratio (RER) of >1.1; and (3) an age-predicted heart rate of ≥85% [27, 28]. At the point of exhaustion, the workload was immediately decreased to 20 W and participants engaged in a 3 min active recovery phase before completing a final 3 min passive recovery period. To ensure a reasonably similar exercise duration between participants, the per-minute incremental increases in workload occurred at 15 W (n=45, 100% CAN, 88% NO CAN), 20 W (n=1, NO CAN) or 25 W (n=2, NO CAN), depending on participants’ habitual physical activity patterns as determined via the International Physical Activity Questionnaire and a conversation with the research team (total METS [metabolic equivalents, min/week]: CAN 2912.4 ± 2522.9 vs NO CAN 2397.2 ± 2213.4, p=0.461).
GXT measurements
During exercise, breath-by-breath data were measured using a pulmonary gas analyser (Vyntus ONE; Vyaire medical, IL, USA) calibrated using certified gases (Gas 1, ambient air; Gas 2, 15% O2, 5% CO2) with data displayed for standardised temperature and pressure for dry air. Integrated heart rate (HR) data were recorded continuously via chest belt telemetry (Polar Electro, Finland). Raw cardiopulmonary data were exported in intervals of 5 s (SentrySuite software; Vyaire medical) and subsequently averaged in segments of 30 s for statistical processing.
The peak rate of O2 consumption (\({\dot{V}\text{O}}_{2\text{peak}}\)) was defined as the highest volume of O2 uptake (l/min) obtained in the 30 s prior to the peak workload achieved. \({\dot{V}\text{O}}_{2\text{peak}}\) was used rather than \({\dot{V}\text{O}}_{2\text{max}}\) due to an inability to identify a plateau in some participants’ O2 consumption rates because of the short duration of the exercise test and/or volitional termination occurring rapidly upon attainment of peak power. All other cardiopulmonary and performance variables were indexed to the \({\dot{V}\text{O}}_{2\text{peak}}\) value. The anaerobic threshold (AT) was computed as the second ventilatory threshold (VT2) and all other cardiopulmonary variables were time-referenced against the indexed volume of O2 uptake (\({\dot{V}\text{O}}_{2}\)).
Laboratory analyses of blood samples
Venous-derived blood samples were obtained at rest, every 3 min during GXT, at the point of volitional exhaustion and during the active and passive recovery periods. An aliquot (300 µl) of blood was centrifuged at 10,552 g for 30 s and the resultant supernatant fraction (plasma) was processed immediately via the YSI 2500 Biochemistry Analyser (YSI Ohio, USA) to determine point concentrations of PG and plasma lactate (PLa). The remaining sample was centrifuged and stored at −80°C for subsequent analyses of catecholamines (adrenaline [epinephrine] and noradrenaline [norepinephrine]) using ELISA kits (EA613/192, Eagle biosciences, Nashua, NH, USA).
Statistical analyses
For identifying differences in point-value numerical data between groups Student’s t test was used with two-tailed p values reported for significance. Differences between categorical variables were assessed via the χ2 test unless more than 20% of cells had expected frequencies <5, in which case the Fisher exact test was used. A two-way repeated-measures ANOVA with Bonferroni-corrected pairwise comparisons was used to compare between-group differences in acute metabolic, cardiopulmonary and sympathoadrenal system responses to GXT. Interaction effects were reported with main and simple effects followed up in post hoc analyses. In instances where sphericity was violated and the Greenhouse–Geisser ε value was >0.750, Huynh–Feldt results were reported. The Pearson correlation coefficient was used to establish the strength of association between metabolic cardiopulmonary and sympathoadrenal system responses. Simple linear regression was conducted to evaluate the predictive power of selected physiological variables (CRF and HR) on the sympathoadrenal system responsivity to GXT. Raw \({\dot{V}\text{O}}_{2}\) data were expressed in METs (i.e. 1-MET approximates the amount of oxygen consumed while sitting at rest and is equal to 3.5 ml O2 [kg body weight]−1 min−1). The difference between actual vs predicted oxygen uptake (\({\dot{V}\text{O}}_{2\text{peak}}\) predicted) was calculated via the equations proposed by the FRIEND registry database [29]. The amount of time spent with PG within a specific glucose zone was calculated as the number of PG readings that fell within that zone divided by the total number of PG readings from the participant, represented as a percentage (i.e. time below range <3.9 mmol/l [<70 mg/dl]), time in range 3.9–10.0 mmol/l [70–180 mg/dl]), time above range >10.0 mmol/l [>180 mg/dl]) [30]. Indexes of glycaemic variability included the SD and CV. All statistical analyses were done using SPSS Version 29.0.1.0(171) (IBM SPSS Statistics); α was set at 0.05 and statistical significance was accepted when p≤0.05.
Results
Participant characteristics
A total of 48 participants (split into 24 matched pairs; 7 female, 17 male) completed the study. Baseline characteristics of the included cohort when stratified into their respective CAN groupings are displayed in Table 1.
The number of people in the NO CAN group who attained the target HbA1c level of ≤53 mmol/mol (7%) was almost triple that in the CAN group (NO CAN n=14 vs CAN n=5, χ2 [1, n=48]=7.056, p=0.008).
Information on medical treatments in both groups can be found in electronic supplementary material (ESM) Table 1. For the insulin treatment modality (injection vs insulin pump) and antihypertensive treatment (percentage and type of drug), there were no differences between the two groups. Twenty-nine per cent of the participants with CAN received antidepressants while none did so in the NO CAN group (p=0.009).
Cardiopulmonary responses and exercise performance variables
The grouped mean cardiopulmonary and exercise performance variables in response to GXT at both the AT and peak exercise workloads are presented in Table 2.
The CAN group demonstrated significantly lower \({\dot{V}\text{O}}_{2}\) values when expressed in absolute and relative terms as well as when indexed against reference predicted values at both the AT and peak workloads (Table 2). This was corroborated by reduced power output and duration of exercise at both intensity domains as well as impairments in several cardiorespiratory parameters with increasing exercise intensity (i.e. \({\dot{V}\text{CO}}_{2}\), HR, ventilatory equivalents and breathing frequency; Table 2).
Data were also reanalysed to account for differences in external work rate between the two groups. Table 3 presents the cardiopulmonary data when participants with CAN were matched to those without CAN based on a similar peak external workload. Each CAN participants’ peak load was used as the reference point from which the corresponding load-matched data taken from a NO CAN participant was paired (ranked in ascending order of peak wattage). The CAN \({\dot{V}\text{O}}_{2\text{peak}}\) value represented 83.9 ± 9.3% of that for the NO CAN cohort.
Sympathoadrenal system responses
Adrenaline
Figure 1a details plasma adrenaline concentrations during GXT in both groups. A significant interaction effect was found between CAN status and adrenaline concentrations over time (F [1.264, 51.837]=9.559, p=0.002). Adrenaline concentrations were higher in the NO CAN group both at peak workload (NO CAN 0.38 ± 0.27 ng/ml vs CAN 0.17 ± 0.12 ng/ml, p=0.002) and at recovery 15 min after test cessation (NO CAN 0.08 ± 0.04 vs CAN 0.04 ± 0.05 ng/ml, p=0.010). Peak adrenaline concentrations were significantly elevated from all other timepoints in both groups (NO CAN, all within-condition differences p<0.001; CAN, all within-condition differences p≤0.02). The magnitude of change in adrenaline concentrations from rest to peak workload was ~84% greater in the NO CAN group (NO CAN Δ +0.32 ± 0.24 ng/ml vs CAN Δ +0.13 ± 0.12 ng/ml, p=0.005).
Plasma adrenaline (a) and noradrenaline (b) concentrations at various GXT stages, as well as their respective correlation with \({\dot{V}\text{O}}_{2\text{peak}}\) values when expressed as a change from rest to peak workload (c, d) and the corresponding change in HR from rest to peak (e, f). In (a, b) white circles and squares represent a significant difference in the point concentration of a biomarker relative to the within-cohort value taken at rest (i.e. before commencing exercise). *p≤0.05 for CAN vs NO CAN point concentration of a biomarker. Data are presented as mean ± SEM
Simple linear regression analysis was conducted to evaluate the extent to which CRF, as quantified via \({\dot{V}\text{O}}_{2\text{peak}}\) (ml kg−1 min−1), could predict the magnitude of change in adrenaline from rest to peak workload. A significant regression was found (F [1, 41]=20.323, p<0.001, R2=0.332, Fig. 1c), with the indication that for each 1 ml min−1 kg−1 increase in \({\dot{V}\text{O}}_{2\text{peak}}\), the change in adrenaline increased by ~0.016 ng/ml (95% CI 0.009, 0.023]). Strong positive correlations were also found between the degree of increase in change in HR and adrenaline (r[42]=0.551, p<0.001, Fig. 1e).
Noradrenaline
Figure 1b provides a graphical illustration of plasma noradrenaline concentrations at the four pre-identified timepoints during GXT in both groups. A significant interaction effect was found between CAN status and noradrenaline concentrations over time (F [1.450, 58.018]=7.234, p=0.004). Noradrenaline concentrations were higher in the NO CAN group at the peak workload (NO CAN 2.85 ± 1.23 vs CAN 1.86 ± 1.04 ng/ml, p=0.007) but were comparable at all other stages. Peak noradrenaline concentrations were significantly elevated from all other timepoints in both groups (NO CAN, all-within condition differences p<0.001; CAN, all within-condition differences, p<0.001). The magnitude of change in noradrenaline from rest to peak workload was ~55% greater in the NO CAN group (NO CAN Δ +2.33 ± 1.30 ng/ml vs CAN Δ +1.33 ± 0.89 ng/ml, p=0.005).
Peak aerobic rate was considered a significant predictor of the change in noradrenaline from rest to peak (F[1, 40]=9.134, p=0.004, R2=0.186, Fig. 1d). For each 1 ml min−1 kg−1 increase in \({\dot{V}\text{O}}_{2\text{peak}}\), the change in noradrenaline increased by ~0.067 ng/ml (95% CI 0.022, 0.112). Strong positive correlations were also found between the degree of increase in change in heart rate and noradrenaline (r[41]=0.529, p<0.001, Fig. 1f).
PG responses
Figure 2a displays the PG responses throughout and acutely after GXT in both groups. No interaction effect was found, nor was there any evidence that CAN status influenced PG responses to GXT in main effects follow-up (F [1, 44]=1.200, p=0.279). In both groups, PG concentrations measured at each stage of the GXT remained stable and equivalent to those taken at the respective rested workload.
PG (a) and PLa (b) concentrations at various stages of GXT. White circles and squares represent a significant difference in the point concentration of a biomarker relative to the within-cohort value taken at rest (i.e. before commencing exercise). *p≤0.05 for CAN vs NO CAN point concentration of a biomarker. Data are presented as mean ± SEM
The change in PG from the start (rest) to end (i.e. after a 3 min passive recovery phase) of GXT was similar between groups (NO CAN Δ+0.24 ± 1.24 mmol/l vs CAN Δ+0.01 ± 0.75 mmol/l, p=0.445). A proportionate number of participants experienced an increase in PG over exercise in each group (NO CAN, n=13 [54%] vs CAN, n=14 [58%], χ2 [1, n=48]=0.085, p=0.771).
Table 4 displays glycaemic variables for both groups from exercise onset to 15 min after GXT cessation.
PLa responses
Figure 2b displays the PLa responses to GXT in both groups. There was a significant time × condition interaction effect in PLa responses (F [1.568, 68.994]=6.524, p=0.005). PLa concentrations were higher in the NO CAN group at the peak (NO CAN 5.4 ± 2.1 mmol/l vs CAN 4.0 ± 1.6 mmol/l, p=0.018), dynamic cool down (NO CAN 7.3 ± 2.8 mmol/l vs CAN 5.3 ± 1.9 mmol/l, p=0.007) and end of exercise (NO CAN 7.4 ± 2.8 mmol/l vs CAN 5.4 ± 2.0 mmol/l, p=0.009) timepoints, with a statistically non-significant elevation 15 min after exercise cessation (Δ +1.01 ± 3.6 mmol/l, p=0.064). PLa concentrations were raised from rested concentrations at each stage of GXT from the AT timepoint onwards in both groups.
CAN demonstrated an attenuation in the magnitude of rise in PLa during GXT from rest to end compared with NO CAN (NO CAN Δ +6.4 ± 2.7 mmol/l vs CAN Δ +4.4 ± 1.9 mmol/l, p=0.007).
Discussion
This study profiled the cardiopulmonary, sympathoadrenal system and metabolic responses to GXT in an age-, sex- and BMI-matched cohort of adults with type 1 diabetes with and without CAN. The presence of CAN was associated with the following: (1) lower functional capacity and exercise tolerance characterised by attenuations in several cardiopulmonary responses across the exercise intensity spectrum; (2) impaired sympathoadrenal system responses to maximal effort exercise; (3) a lower PLa profile from the AT onwards; and (4) stable and similar glycaemic responses throughout the exercise test.
Cardiopulmonary findings
Our findings demonstrate that CAN was associated with significantly lower rates of O2 consumption (\({\dot{V}\text{O}}_{2}\)) expressed in absolute or relative values or when indexed against predicted values at both submaximal (AT) or maximal (\({\dot{V}\text{O}}_{2\text{peak}}\)) workload domains (Table 2). Indeed, in those with CAN, \({\dot{V}\text{O}}_{2\text{peak}}\) was reduced by 34% (7.85 ml min−1 kg−1 or 2.2 METs) and quantifiably more individuals with the condition failed to achieve a \({\dot{V}\text{O}}_{2\text{peak}}\) of >30 ml min−1 kg−1 (CAN n=23 vs NO CAN n=15, χ2 [1, n=48]=8.084, p=0.004), a reference standard using the 50th percentile for adults within our study cohort age range [31]. While only one participant in the NO CAN group had a \({\dot{V}\text{O}}_{2\text{peak}}\) that fell below <5 METs, the number of people for whom this was the case in CAN was tenfold higher (χ2 [1, n=48]=9.553, p=0.002). On the other hand, no participant with CAN achieved a \({\dot{V}\text{O}}_{2\text{peak}}\) >10 METs, yet four individuals without CAN surpassed this threshold (Fisher’s exact test, p=0.109).
Numerous global research trials have documented the importance of CRF as a predictor of all-cause and CVD mortality among clinically referred populations. A meta-analysis by Kodama et al consisting of 33 studies and nearly 103,000 participants showed that, compared with participants in the most fit tertile, those with low CRF had a 70% and 56% higher risk for all-cause and cardiovascular mortality, respectively [10]. Across all studies, a 13% and 15% reduction in cardiovascular and all-cause mortality, respectively, was observed per 1-MET increase in exercise capacity [10]. In a recent update report, the findings were further reinforced [9] and have been consistently backed by other large meta-analyses with participant numbers in the multi-millions [11]. Data of this nature have given rise to the advocacy for routine GXT as a ‘vital sign’ in clinical practice by several leading scientific cardiac committees/associations in both the USA and Europe [32,33,34,35]. Importantly, the greatest mortality benefits occur when progressing from the least fit to the next ‘least fit’ group [36, 37], hence the emphasis on increasing physical activity in those with low CRF [25]. Considering the 2-MET deficit in those with type 1 diabetes and CAN noted in our study, a targeted approach in this cohort where intensified efforts are made to improve CRF by even small increments (as little as 1-MET), may have profound benefit in reducing an already elevated CVD risk profile. Worth considering when interpreting findings is the methodological differences in determining CRF across literature (e.g. whether aerobic capacity is reported as a true maximum / peak oxygen intake or a predicted value using submaximal testing).
The present study also demonstrates that the condition of CAN when superimposed on type 1 diabetes was associated with lower minute ventilation and breathing frequency at the peak exercise workload. A low peak breathing reserve may signal a demand/capacity imbalance of the respiratory system; this is an important mechanism of exertional dyspnoea. During light- to moderate-intensity exercise (up to ≈55% \({\dot{V}\text{O}}_{2\text{max}}\)), ventilation increases linearly with oxygen consumption and carbon dioxide production, averaging around 20–25 l of air per litre of oxygen consumed. Fittingly, both our study cohorts fell within this bracket, with grouped means of ≈25 l at AT. Under these conditions, increases in ventilation are driven mainly by increases in tidal volume (i.e. the depth of breathing), whereas at higher exercise intensities, increases in breathing frequency predominate. Interestingly, this transpired in our data, whereby even though ventilation was lower at the AT (≈55% \({\dot{V}\text{O}}_{2\text{peak}}\) in both of our study cohorts), both the VE/\({\dot{V}\text{O}}_{2}\) and breathing frequency were almost identical between groups. It was only when exercise intensity progressed that both ventilation and breathing frequency were impaired in those with CAN, with evidence of this impacting VE/\({\dot{V}\text{O}}_{2}\).
The time to reach both the AT and peak exercise workloads was shorter in the CAN group (by 13% and 15%, respectively; Table 2). This was coupled with a reduced power output at both exercise intensity domains (by 38% and 27%, respectively, Table 2). Though the absolute workload (defined as the power output in W) at which participants exercised at the AT was proportionately lower in those with CAN (by 38%), the relativised exercise intensity (defined as a % of attained \({\dot{V}\text{O}}_{2\text{peak}}\)) at which they did so was higher (by 12%) than those without CAN. Yet, despite significant differences in both external mechanical workload and several cardiopulmonary variables between groups at the AT and peak exercise intensity domains, the subjective perception of effort was similar between groups. These findings align with early work by Hilsted et al [19], whereby comparable ratings of perceived exertion during GXT were noted in juveniles with diabetes with and without neuropathy.
Like Hilsted et al [19], we also found an elevated resting HR in our participants with CAN, supporting the notion of a defective vagal efferent baroreflex pathway. During GXT, our data revealed that a proportionately higher number of participants with CAN failed to achieve ≥85% of their corresponding age-predicted maximal HR compared with those without CAN ([i.e. 220 − age] n=14 vs n=2, respectively, χ2 [1, n=47]=12.888, p<0.001). This was corroborated by a significantly lower HR reserve in the CAN cohort, with the difference between resting and peak values in the CAN cohort being ≈27 beats/min lower for HR, ≈20 beats/min smaller for HRpeak and ≈2 ml per beats/min smaller for O2 pulsepeak. In the transition from rest to maximal exercise, increases in HR rely on reciprocal antagonism of the parasympathetic and sympathetic branches of the autonomic nervous system [38]. Indeed, increases in HR during progressive exercise workloads transition from a 4:1 vagal–sympathetic balance at rest to a 4:1 sympatho–vagal balance at higher intensity workloads [38]. Interestingly, we noticed a distinct cross-over profile in HR dynamics between groups wherein despite initially elevated HR values at rest (NO CAN 74 ± 10 beats/min vs CAN 81 ± 11 beats/min, p=0.021), values equalled out during the early phases of exercise (i.e. the warm-up [NO CAN 84 ± 13 beats/min vs CAN 90 ± 10 beats/min, p=0.141] and the AT; Table 2) but then became significantly lower as exercise intensity progressed towards peak (14% lower; Table 2). Hence, it appears that in individuals with type 1 diabetes and CAN, greater sympathetic dominance presides at rest and the deficiency of the sympathetic autonomic system outflow may be the main driver preventing an adequate cardiovascular response to higher-intensity exercise. Fittingly, we saw strong positive correlations between the degree of change from rest to peak exercise workload in plasma catecholamines and HR (Fig. 1e, f).
Sympathoadrenal system findings
Adults with type 1 diabetes and CAN presented with significantly lower absolute plasma catecholamine concentrations at peak exercise coupled with an attenuation in the magnitude of increase from rest to peak values (ΔRest–Peak). These findings align with those of others who have reported impaired cardiovascular and sympathoadrenal system responses to GXT in individuals with diabetes and autonomic system dysfunction relative to those without evidence of autonomic dysfunction [39, 40]. The mechanisms driving the blunted sympathoadrenal system response in individuals with CAN may reflect the pathophysiological hallmarks of the condition due to damage to motor nerve fibres, metaboreceptor and/or mechanoreceptor fibres and/or pre/post-ganglionic nerve fibres. Worth noting was the uncontrolled use of concomitant medications by our participants, as some of those medications can exert modulatory effects on the cardiovascular system. Indeed, antidepressant treatment was used solely by individuals in our CAN cohort. Our clinical records revealed that two different classes of drugs were used, with a reported possible 1–10% increase in HR as a potential side effect. Though our regression analyses found no evidence of their use affecting our primary outcome (i.e. \({\dot{V}\text{O}}_{2\text{peak}}\)), it certainly warrants consideration and calls into question the appropriateness of utilising some of the conventional variables provided by GXT (e.g. HR) for exercise prescriptive purposes in those with type 1 diabetes and CAN.
Metabolic findings
Glucose
Plasma glucose did not differ between groups, nor did it deviate from the pre-exercise concentration at any point during GXT. These observations are in keeping with findings across various in-house studies involving participants with type 1 diabetes using identical preparatory procedures and exercise test protocols (pooled mean across three separate studies: Δ −0.1 ± 0.3 mmol/l) [20, 21, 41]. Hence, at least when the current GXT procedure is followed, it does not seem to matter whether one’s insulin regimen is that of injection therapy [20] or pump [21], whether the latter is a pump with non-automated vs automated features [21], or indeed which type of automated insulin delivery system it is, if it is one [41]. It also does not appear to matter if one is older (as per the present study), adolescent [41], male or female [41]; glucose concentrations are unlikely to change during GXT in those with type 1 diabetes. This glycaemic profile may reflect the counterbalance between the initial increase in the rate of intramuscular glucose uptake at lower-intensity exercise with its accelerated release (from both glycogenolysis and gluconeogenesis) as exercise intensity progresses.
Though GXT represents a physiological ‘stressor’, its relatively brief duration and progressive intensity are unlikely to prompt a rapid decline in blood glucose, providing a plausible explanation for the equivalency in PG throughout exercise between the groups. When coupled with the preparatory procedures put in place ahead of test performance in the current study (i.e. the minimisation of overt hyperinsulinaemia by the avoidance of bolus insulin within 2 h before laboratory attendance; the avoidance of antecedent hypoglycaemia and strenuous physical activity in the 24 h prior to testing; and a starting threshold in PG of >5 mmol/l to provide somewhat of a safety blanket from which any drops in PG could be caught early in our 3 min sampling schedule), there may be a reduced risk of hypoglycaemia.
Lactate
PLa concentrations were significantly lower in the CAN group at each stage of the GXT from the AT onwards. The β-adrenergic system, principally adrenaline, stimulates muscle glycogenolysis, leading to an increase in the rate of glycolytic flux and, hence, lower lactate production. We, like others, also observed associations between catecholamines and lactate concentration increases during progressive maximal exercise [42,43,44]. Indeed, in our data, the magnitude of change from rest to peak (ΔRest−Peak) in both adrenaline (r[43]=0.659, p<0.001) and noradrenaline (r[42]=0.419, p=0.006) were highly and positively correlated with ΔRest–Peak in lactate. During progressive exercise, with developing lactic acidosis, ventilation increased markedly to compensate for exercise-induced metabolic acidosis. Interestingly, minute ventilation only increased 2.8-fold from AT to peak workload in those with CAN but 4.4-fold in those with NO CAN.
Strengths, limitations and future directions
This study matched adults with type 1 diabetes with or without CAN and profiles the sympathoadrenal, metabolic and cardiovascular responses to incremental, maximal exercise testing. The information within may help provide a basis from which targeted interventions aimed at reducing the development and/or progression of diabetes-related complications can be formulated. Important limiting factors of this study are the uncontrolled use of concomitant medications, some of which may have influenced test outcomes, and differences in diabetes and/or anthropometric variables between groups. Consideration for the fact that a high percentage of our cohort had adult-onset type 1 diabetes should also be exercised. Longitudinal monitoring of CRF alongside changes in complication status as well as interventions investigating the influence of regular exercise training on the pathogenesis of CAN in those with type 1 diabetes would be insightful considerations for future research incentives.
Conclusion
This study demonstrated that in adults with type 1 diabetes, CAN was associated with exercise intolerance characterised by impairments in various cardiopulmonary, sympathoadrenal system and metabolic responses to GXT. These data support uncovering the presence of CAN when prescribing a personalised physical training plan.
Abbreviations
- AT:
-
Anaerobic threshold
- CAN:
-
Cardiovascular autonomic neuropathy
- CART:
-
Cardiovascular reflex test
- CRF:
-
Cardiorespiratory fitness
- GXT:
-
Graded exercise testing
- HR:
-
Heart rate
- MET:
-
Metabolic equivalents
- PG:
-
Plasma glucose
- PLa:
-
Plasma lactate
- RER:
-
Respiratory exchange ratio
- VT2:
-
Second ventilatory threshold
References
Mizrak HI, Kufaishi H, Hecquet SK et al (2024) Contemporary prevalence of diabetic neuropathies in individuals with type 1 and type 2 diabetes in a Danish tertiary outpatient clinic. J Diabetes Complications 38(6):108761. https://doi.org/10.1016/J.JDIACOMP.2024.108761
Vinik AI, Erbas T, Casellini CM (2013) Diabetic cardiac autonomic neuropathy, inflammation and cardiovascular disease. J Diabetes Investig 4(1):4–18. https://doi.org/10.1111/JDI.12042
Chowdhury M, Nevitt S, Eleftheriadou A et al (2021) Cardiac autonomic neuropathy and risk of cardiovascular disease and mortality in type 1 and type 2 diabetes: a meta-analysis. BMJ Open Diabetes Res Care 9(2):e002480. https://doi.org/10.1136/BMJDRC-2021-002480
Voulgari C, Papadogiannis D, Tentolouris N (2010) Diabetic cardiomyopathy: from the pathophysiology of the cardiac myocytes to current diagnosis and management strategies. Vasc Health Risk Manag 6(1):883–903. https://doi.org/10.2147/VHRM.S11681
Roy TM, Peterson HR, Snider HL et al (1989) Autonomic influence on cardiovascular performance in diabetic subjects. Am J Med 87(4):382–388. https://doi.org/10.1016/S0002-9343(89)80818-6
Duncker DJ, Bache RJ (2008) Regulation of coronary blood flow during exercise. Physiol Rev 88(3):1009–1086. https://doi.org/10.1152/PHYSREV.00045.2006
Albouaini K, Egred M, Alahmar A, Wright DJ (2007) Cardiopulmonary exercise testing and its application. Postgrad Med J 83(985):675. https://doi.org/10.1136/HRT.2007.121558
Levett DZH, Jack S, Swart M et al (2018) Perioperative cardiopulmonary exercise testing (CPET): consensus clinical guidelines on indications, organization, conduct, and physiological interpretation. Br J Anaesth 120(3):484–500. https://doi.org/10.1016/j.bja.2017.10.020
Harber MP, Kaminsky LA, Arena R et al (2017) Impact of cardiorespiratory fitness on all-cause and disease-specific mortality: advances since 2009. Prog Cardiovasc Dis 60(1):11–20. https://doi.org/10.1016/J.PCAD.2017.03.001
Kodama S, Saito K, Tanaka S et al (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301(19):2024–2035. https://doi.org/10.1001/JAMA.2009.681
Lang JJ, Prince SA, Merucci K et al (2024) Cardiorespiratory fitness is a strong and consistent predictor of morbidity and mortality among adults: an overview of meta-analyses representing over 20.9 million observations from 199 unique cohort studies. Br J Sports Med 58(10):556–566. https://doi.org/10.1136/BJSPORTS-2023-107849
American Thoracic Society/American College of Chest Physicians (2003) ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 167:211–277
Komatsu WR, Gabbay MAL, Castro ML et al (2005) Aerobic exercise capacity in normal adolescents and those with type 1 diabetes mellitus. Pediatr Diabetes 6(3):145–149. https://doi.org/10.1111/j.1399-543X.2005.00120.x
Komatsu WR, Neto TLB, Chacra AR, Dib SA (2010) Aerobic exercise capacity and pulmonary function in athletes with and without type 1 diabetes. Diabetes Care 33(12):2555–2557. https://doi.org/10.2337/DC10-0769
Eckstein ML, Farinha JB, McCarthy O et al (2021) Differences in physiological responses to cardiopulmonary exercise testing in adults with and without type 1 diabetes: a pooled analysis. Diabetes Care 44(1):240–247. https://doi.org/10.2337/DC20-1496
Williams BK, Guelfi KJ, Jones TW, Davis EA (2011) Lower cardiorespiratory fitness in children with Type 1 diabetes. Diabet Med 28(8):1005–1007. https://doi.org/10.1111/J.1464-5491.2011.03271.X
Peltonen JE, Koponen AS, Pullinen K et al (2012) Alveolar gas exchange and tissue deoxygenation during exercise in type 1 diabetes patients and healthy controls. Respir Physiol Neurobiol 181(3):267–276. https://doi.org/10.1016/J.RESP.2012.04.002
Hägglund H, Uusitalo A, Peltonen JE et al (2012) Cardiovascular autonomic nervous system function and aerobic capacity in type 1 diabetes. Front Physiol 3:356. https://doi.org/10.3389/FPHYS.2012.00356
Hilsted J, Galbo H, Christensen NJ (1979) Impaired cardiovascular responses to graded exercise in diabetic autonomic neuropathy. Diabetes 28(4):313–319. https://doi.org/10.2337/DIAB.28.4.313
McCarthy O, Pitt J, Wellman BEN et al (2021) Blood glucose responses during cardiopulmonary incremental exercise testing in type 1 diabetes: a pooled analysis. Med Sci Sports Exerc 53(6):1142–1150. https://doi.org/10.1249/MSS.0000000000002584
McCarthy OM, Birch Kristensen K, Bechmann Christensen M et al (2023) Metabolic and physiological responses to graded exercise testing in individuals with type 1 diabetes using insulin pump therapy. Diabetes Obes Metab 25(3):878–888. https://doi.org/10.1111/DOM.14938
Meyer C, Großmann R, Mitrakou A et al (1998) Effects of autonomic neuropathy on counterregulation and awareness of hypoglycemia in type 1 diabetic patients. Diabetes Care 21(11):1960–1966. https://doi.org/10.2337/DIACARE.21.11.1960
Koivikko ML, Salmela PI, Airaksinen KEJ et al (2005) Effects of sustained insulin-induced hypoglycemia on cardiovascular autonomic regulation in type 1 diabetes. Diabetes 54(3):744–750. https://doi.org/10.2337/DIABETES.54.3.744
Spallone V (2019) Update on the impact, diagnosis and management of cardiovascular autonomic neuropathy in diabetes: what is defined, what is new, and what is unmet. Diabetes Metab J 43(1):3–30. https://doi.org/10.4093/DMJ.2018.0259
Cisternas NS (2018) ACSM guidelines for exercise testing and prescription, 10th edn. Wolters Kluwer Health, Philadelphia, PA
Clarke WL, Cox DJ, Gonder-Frederick LA, Julian D, Schlundt MD, Polonsky W (1995) Reduced awareness of hypoglycemia in adults with IPPM A prospective study of hypoglycemic frequency and associated symptoms. Diabetes Care 18(4):517–22. https://doi.org/10.2337/diacare.18.4.517
Moser O, Eckstein ML, Mueller A et al (2019) Reduction in insulin degludec dosing for multiple exercise sessions improves time spent in euglycaemia in people with type 1 diabetes: a randomised cross-over trial. Diabetes Obes Metab 21(2):349–356. https://doi.org/10.1111/dom.13534
Hofmann P, Tschakert G (2011) Special needs to prescribe exercise intensity for scientific studies. Cardiol Res Pract 2011:209302. https://doi.org/10.4061/2011/209302
Myers J, Kaminsky LA, Lima R, Christle JW, Ashley E, Arena R (2017) A reference equation for normal standards for VO2 Max: analysis from the Fitness Registry and the Importance of Exercise National Database (FRIEND Registry). Prog Cardiovasc Dis 60(1):21–29. https://doi.org/10.1016/J.PCAD.2017.03.002
Battelino T, Danne T, Bergenstal RM et al (2019) Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 42(8):1593–1603. https://doi.org/10.2337/dci19-0028
Kaminsky LA, Arena R, Myers J (2015) Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing: data from the fitness registry and the importance of exercise national database. Mayo Clin Proc 90(11):1515–1523. https://doi.org/10.1016/J.MAYOCP.2015.07.026
Arena R, Myers J, Williams MA et al (2007) Assessment of functional capacity in clinical and research settings: a scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation 116(3):329–343. https://doi.org/10.1161/CIRCULATIONAHA.106.184461
Mezzani A, Agostoni P, Cohen-Solal A et al (2009) Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: a report from the Exercise Physiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 16(3):249–267. https://doi.org/10.1097/HJR.0B013E32832914C8
Gibbons RJ, Balady GJ, Beasley JW et al (1997) ACC/AHA guidelines for exercise testing: a report of the american college of Cardiology/American Heart Association task force on practice guidelines (Committee on Exercise Testing). J Am Coll Cardiol 30(1):260–311. https://doi.org/10.1016/S0735-1097(97)00150-2
Balady GJ, Arena R, Sietsema K et al (2010) Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American heart association. Circulation 122(2):191–225. https://doi.org/10.1161/CIR.0B013E3181E52E69
Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE (2002) Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 346(11):793–801. https://doi.org/10.1056/NEJMOA011858
Blair S, Kohl H, Paffenbarger R, Clark D, Cooper K, Gibbons L (1989) Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 262(17):2395–2401. https://doi.org/10.1001/JAMA.262.17.2395
White DW, Raven PB (2014) Autonomic neural control of heart rate during dynamic exercise: revisited. J Physiol 592(Pt 12):2491. https://doi.org/10.1113/JPHYSIOL.2014.271858
Bottini P, Tantucci C, Scionti L et al (1995) Cardiovascular response to exercise in diabetic patients: influence of autonomic neuropathy of different severity. Diabetologia 38(2):244–250. https://doi.org/10.1007/BF00400101
Kasahara Y, Izawa K, Omiya K et al (2006) Influence of autonomic nervous dysfunction characterizing effect of diabetes mellitus on heart rate response and exercise capacity in patients undergoing cardiac rehabilitation for acute myocardial infarction. Circ J 70(8):1017–1025. https://doi.org/10.1253/CIRCJ.70.1017
Lindkvist EB, McCarthy OM, Tawfik S et al (2025) Glycemic responses to graded exercise testing in adolescents using automated insulin delivery systems. Diabetes Technol Ther. https://doi.org/10.1177/15209156251390834
Schneider DA, McLellan TM, Gass GC (2000) Plasma catecholamine and blood lactate responses to incremental arm and leg exercise. Med Sci Sports Exerc 32(3):608–613. https://doi.org/10.1097/00005768-200003000-00009
Mazzeo RS, Marshall P (1989) Influence of plasma catecholamines on the lactate threshold during graded exercise. J Appl Physiol (1985) 67(4):1319–1322. https://doi.org/10.1152/JAPPL.1989.67.4.1319
Turner MJ, Howley ET, Tanaka H, Ashraf M, Bassett DR, Keefer DJ (1995) Effect of graded epinephrine infusion on blood lactate response to exercise. J Appl Physiol 79(4):1206–1211. https://doi.org/10.1152/JAPPL.1995.79.4.1206
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
The authors would like to thank the participants for their willingness to contribute and commit to the study protocol.
Data availability statement
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
OMc, RBB, CSH, RMB and KN contributed to the conception and design of the study. OMc, RBB, ST, SBL, EBL and SHN contributed to the acquisition of data. OMc, ST and RMB were responsible for data analyses. All authors were responsible for data interpretation. OMc wrote the original draft of the manuscript. All authors contributed to revising the article. All authors provided final approval of the version to be published. KN is responsible for the integrity of the work as a whole.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Richard M. Bracken and Kirsten Nørgaard assume shared last author status.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
McCarthy, O.M., Brødsgaard, R.B., Tawfik, S. et al. Impact of cardiovascular autonomic neuropathy on cardiopulmonary, sympathoadrenal and metabolic responses to physical exercise in adults with type 1 diabetes. Diabetologia (2025). https://doi.org/10.1007/s00125-025-06619-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1007/s00125-025-06619-9